Laparoscopic Sleeve Gastrectomy (LSG)
The laparoscopic sleeve gastrectomy (LSG) was originally conceived as the first step of a two-staged procedure for performing Roux-en Y Gastric Bypass (RYGBP) in certain higher risk individuals. Over the years, with the use of small bougies (visualize an inflatable curved ruler), the operation was adopted as a primary operation in its own right. LSG is currently the most commonly performed operation in Australia and many other countries internationally.
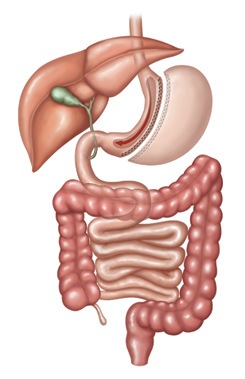
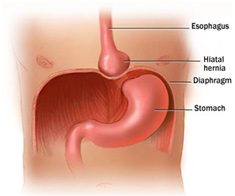
This keyhole operation involves the use of energy devices to help separate the wall of the stomach from the attached blood vessels and nearby structures. If a hiatus hernia is identified at the time of surgery, it is considered best practice for this to be closed/ repaired at the time of surgery.
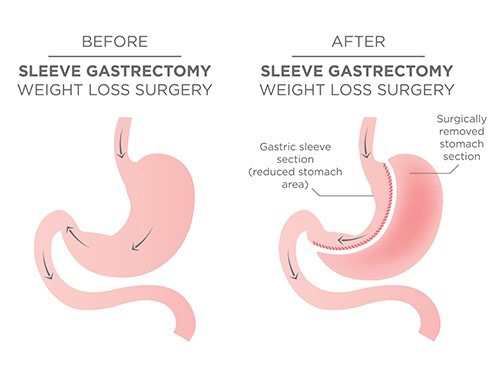
Whilst under general anaesthesia, a bougie is placed through the mouth and slowly introduced into the stomach via the oesophagus. Once inflated by the anesthetist, it acts almost like a curved “ruler” which helps guide the surgeon when cutting approximately 75% of the stomach and applying staples. Most surgeons reinforce the staple line in order to decrease the risk of bleeding and leaks and perform a leak test. The excised (cut away) stomach is then removed from the body via one of the small skin incisions used during the keyhole operation. This makes the operation irreversible ie you can’t change your mind.
Risks & Complications of LSG
The LSG procedure is generally safe, but as with any operation, complications may occur and include but are not limited to:
- Leak at the site of surgery (at the seam) which is uncommon and occurs in 1-2% patients
- Most surgeons reinforce the staple line in order to decrease the risk of bleeding and leaks and perform a leak test.
- It is up to you to follow the “transitional diet” after surgery-as specified by the dietitian, so as to give the seam time to heal (takes approximately 8 weeks to heal)
- Reflux symptoms common and occur in approximately 25% of patients
- This is often managed with medication,
- however, in a small percentage of patients, further surgery may be required to better manage these symptoms (usually the LSG gets converted to a RYGBP)
- Nutritional deficiencies
- Examples include: vitamin B12 deficiency, iron deficiency, low calcium/ vitamin D and sometimes others
- Hence why supplementation with vitamins and minerals, as specified by the dietitian and your treating doctor, must be taken indefinitely
- Gastric sleeve conduit stretches over time
- This may contribute to some of the inevitable weight regain
- Hormonal effects of surgery wear off over the course of a number of years
- This may contribute to some of the inevitable weight regain
- Suboptimal initial-response to Metabolic Bariatric Surgery [MBS]
i.e. unusually modest improvement in a significant obesity-related health condition- Partial-responders vs non-responders to teatment
- At present, there is no pre-operative testing that can be done to determine how you will respond to this or any particular therapy
- However, you might be suitable for add- on therapy eg obesity-modifying medication or a variety of other surgical options